The US National Coordinator for Health Technology defines an Electronic Health Record (EHR) as a digital version of a patient’s paper chart. They contradict themselves on the very next page of their website titled “Benefits of EHR” where they state that it is “more than that”.
Indeed, digitalization has been a buzzword in healthcare a decade or two ago. Now it seems even the most unwilling hospitals aim to use the latest technologies to improve their care.
The same institution states that EHR nowadays at the very least:
- Contains the patient’s medical history, including the meds they’ve been taking, treatment plans, Info about allergies, radiology images, lab test dates, and results, etc.
- Allows access to providers so they can make decisions about patient care
- Automate healthcare providers’ operations and streamline their workflow
The US National Coordinator for Health Technology that EHR use leads to improved patient care, increases their involvement in their well-being, improves care coordination, does good for diagnostics and patient outcomes, and eventually leads to more effective practice and saving costs.
In this article, we’d like to explore a little more which technologies integration makes EHR systems modern and functional these days. The list is quite big and includes various technologies, so we had to handpick the most commonly requested by our clients.
They are Artificial Intelligence, Blockchain, the Internet of Things, Telemedicine, and even Robotic Process Information.
We’ll dive deeper into describing how this or that technology integrated into EHR systems could turn out to help empower this piece of software. In the meantime, you can have a look at our ready-made healthcare solutions case studies employing some of these emerging technologies.
Artificial Intelligence
Healthcare IT News interviewed Sumit Rana, head of research and development at EHR company Epic to figure out how AI could be useful for EHR. Turns out, unsurprisingly, AI could be helpful in more ways than one.
AI could create progress notes, assist with medical coding, and generate draft responses to patients’ questions at the very least. In addition to the fact that AI algorithms can analyze EHR data, recommend treatment plans, and extract and interpret free-text notes within EHRs, we see quite a set of functions!
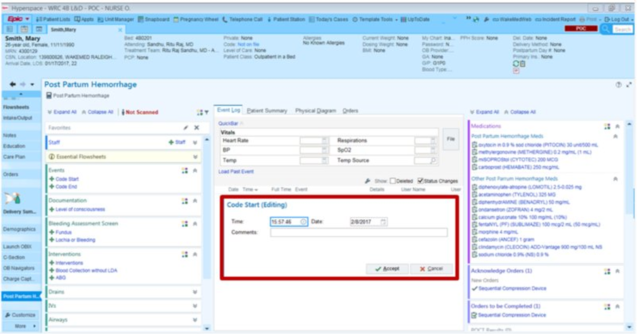
EHR uses AI to generate progress notes from patient/provider conversations in the exam rooms, and Mr. Rana described the process in the following way.
The doctor asks the patient’s permission to record the session, and they do it with the help of their cell phone application. AI can be instructed to make a break in listening if needed, and when the conversation is finished, the software creates a draft of what was discussed. The physician could review and edit the notes, and finalize their documentation.
Epic EHR is a cloud-based software used for these kinds of operations. They proved their effectiveness in the market and gained popularity. If you want to explore ready-made options, we advise checking listings. For tailor-made custom products that cover your specific needs, you can always contact Elinext to get to know how much the development costs.
Source: ehrinpractice.com
As one could guess, this is a time-saving operation. As one of the hospitals reported back to the EHR company, an average time-saving is at 5.5 hours per week, and the doctors see a 76% reduction in time spent after clinic hours, which proves to be significant.
60% of users also reported an increase in documentation quality.
That’s just one installment of AI use. There are plenty of others.
For instance, AI generates a draft response to a patient’s questions. Here is how it looks in practice. When a physician gets a question from a patient (via an app), they see a draft (prepared by AI) waiting for them, and they only have two choices: to alter the draft or to begin answering the message from scratch: a blank text box.
Providers like the AI can pre-browse data in the patient’s chart and already synthesize it for them, so they use the former option more often.
In addition, AI systems learn to communicate with patients in the same way doctors do. So that their messages don’t start with robotic “Dear John”, but rather are held more casually.
We’ve briefly described some of the applications of AI that could be beneficial while being integrated into your EHR. Certainly, there are others. If you’re looking for EHR development that could utilize the full potential of AI, contact us. The chances are that we could partner up to create a great piece of healthcare software.
Blockchain
95% of American hospitals were using EHR systems by 2017. Most of them prefer to be guarded by the blockchain technology.
Several frameworks were designed for remote monitoring of patients and access to their health records, including The Healthcare Blockchain System, or a Smart Contract-Based Framework for Securing Healthcare Data.
Blockchain is a digital database that records healthcare data. A Smart Contract is a piece of executable code that runs on the blockchain without the assistance of a third party. If the criterion is satisfied, actions are taken automatically.
MedRec is one of the companies that uses blockchain for medical data access and permission. For their EHR systems, the Ethereum blockchain network handles a broad set of tasks, such as connecting to the peer-to-peer network, encoding and sending transactions.
Avaneer, a decentralized peer-to-peer network is a platform that aims to bridge gaps in interoperability using a combination of advanced technologies such as AI and blockchain for data transactions and sharing.
Blockchain promises to help EHR unify its standards, increase interoperability, and protect patient privacy, while also helping with data access and sharing.
Internet of Things
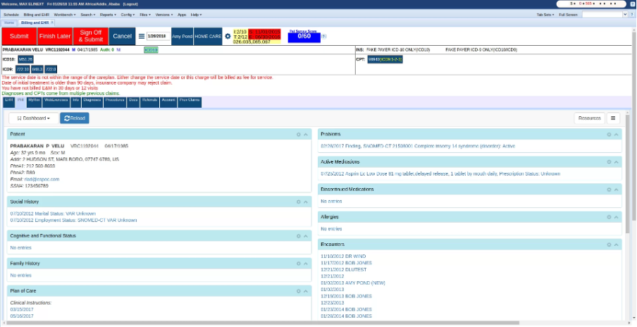
West Health survey states that half of the respondents agree with the fact that patient safety errors may come from the manual transition of data into a chart. More than half of the nurses admit to eye witnessing these patient safety errors. That means, that improvements in medical device interoperability are a must these days.
Medical devices could be linked with a smart network that includes EHR systems — that way the clinical data will be shared across the network and transmitted to EHR directly.
Source: elinext.com
Therefore, the direct connection of medical devices and EHRs reduces the potential for errors related to the manual sharing of information, and that’s a lot in itself.
Cisco Systems, Medtronic, and Qualcomm are three companies in the domain of connected devices, and each of them has over 20 billion in capitalization. They transform the ways the world connects, computes, and communicates.
The global medical device connectivity market size is expected to reach USD 8.49 Billion in 2028 at a CAGR of 24.3% during the forecast period.
The continuous data stream from IoT devices provides EHR systems with timely data and improves the overall patient monitoring quality.
Telemedicine
Well, calling telemedicine an “emerging technology” is a little bit of a stretch. We’re so used to it after the pandemics, it seems the technology has been with us forever. However, we can’t deny that telemedicine could be useful in combination with EHR systems.
Integration of telemedicine with EHRs allows for seamless scheduling, documentation, and follow-up of virtual consultations at the very least.
EHR systems now include remote diagnostic tools that can analyze images or video streams, giving doctors a fuller picture of patient health.
With more accurate and easily accessible patient info, doctors can make better decisions and reduce medical errors.
Better communication and teamwork among healthcare providers lead to more coordinated and patient-focused care. It’s not more complicated than that.
Robotic Process Information
Robotic process automation aka RPA effectively automates patient data entry, and transfer of the info to patient records, and can add relevant meetings to the EHR’s schedule.
Basically, some of the functions of this technology have been described in the previous sections of the current blog post.
Here, we’d like you to get familiarized with how this works in practice. Among the common uses of RPA for EHR are automating revenue cycle, or optimizing scheduling.
Revenue cycle management involves a set of administrative and financial processes to manage the healthcare organization’s revenue stream. For this cycle to operate without any interruptions, many entries have to be correctly implemented. As RPA is integrated, the revenue cycle could be automated effectively, and every tiny error could be corrected in a matter of seconds.
All the processes from Intake to medical billing and invoicing, from payment collection to payment posting run fast as soon as it is automated.
Schedule optimization allows for immediate calculations that consider such factors as client preferences, availability of providers, and billing capacity to be taken into account. That leads to an efficiently optimized schedule.
Conclusion
We’ve explored the ways modern technologies are integrated into EHR in this blog post. As one can see, with the help of AI, blockchain, and other technologies, patient care turns out to be more efficient, secure, and patient-centric.
The market size in the Artificial Intelligence market is projected to reach US$184 billion in 2024. Smart contracts have been used for EHR since 2008. If you’re developing your custom EHR, you should have a vision of which technologies to utilize to provide it’s maximal efficiency.
There are some solutions on the market that would cover most of your needs, but to cover 100% of them you need custom-built software. Elinext is a company that develops EHR powered with different emerging technologies. Contact us to discuss the possibility of cooperation.
However, we keep a close eye on the trends modern EHR systems utilize to improve care, and our custom-made EHRs correspond to the latest standards and use emerging technology capabilities. We’ll elaborate more on the m atter shortly as more and more technologies continue to participate in what. The US National Coordinator for Health Technology calls it “more than a digital version of a patient’s paper chart”.